Macular Hole
Macular hole is an abnormal opening in the center of the macula. Although small, its location in the most sensitive area of the retina can cause substantial loss of vision. Macular holes occur more commonly in females in their 60’s and 70’s, occasionally affecting both eyes. The cause of a macular hole is abnormal traction, or pulling, by the vitreous gel. Occasionally it is a result of trauma. The incidence of macular hole is about 8 people per 100,000 per year. The fellow eye may also develop a macular hole in about 15% of patients. Macular holes usually start small and are initially minimally symptomatic. With time (usually weeks to months), the hole enlarges, making symptoms more noticeable. Taking eye vitamins does not lower the risk for macular hole formation.
Symptoms
Symptoms include decreased central vision, ranging from 20/80 to 20/400 or worse. Due to the location of the macular hole, patients describe a central blind spot, while peripheral vision remains normal. Without treatment, the majority of patients with a macular hole will experience progressive loss of central vision as the hole enlarges.
Evaluation
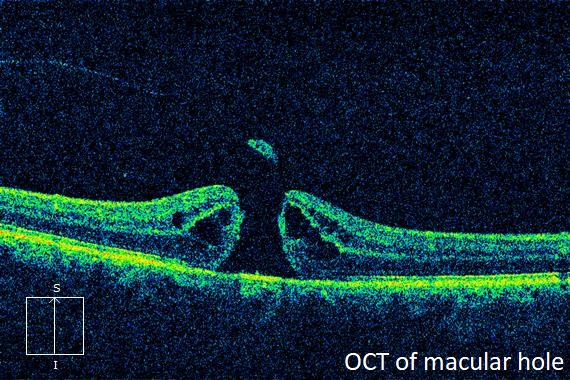
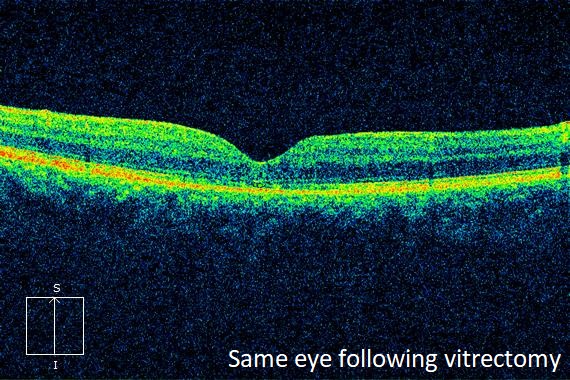
The diagnosis of macular hole is usually made by its characteristic clinical appearance. Optical coherence tomography (OCT), a scanning laser that gives a cross sectional image of the retina, is very useful in confirming the diagnosis. OCT is also useful in detecting vitreous traction, or the presence of macular edema or epiretinal membrane.
Treatment
The mainstay treatment for a macular hole is vitrectomy surgery. During this procedure, the vitreous gel is removed along with the delicate internal limiting membrane (ILM) that pulls, or holds, the macular hole open. Under an operating microscope, the surgery is performed using very fine instruments. Brilliant blue is applied to stain the inner macular surface and highlight membranes present. An absorbable gas bubble is placed in the eye to seal the hole. Depending on the type of gas used, the body will completely absorb the gas bubble within a few weeks to a month or two.
Pars plana vitrectomy
Vitrectomy surgery is an outpatient procedure performed under local anesthesia. Following surgery, most surgeons believe it is crucial for the patient to maintain a downward gaze for one week, keeping the bubble in constant contact with the macular hole, promoting hole closure.
In patients able to comply with face-down positioning, hole closure occurs in almost all cases. Most patients experience a significant improvement in vision following successful macular hole repair.
Complications
The most common complication of vitrectomy, particularly vitrectomy with a gas bubble, is cataract progression. The majority of cataracts occur within a few years of surgery, and many will necessitate cataract extraction.
Other complications include retinal tear (10%) or retinal detachment (1%). Retinal tears, when detected intraoperatively, are treated with laser.
Gas related complications include high or low eye pressure. While there is gas bubble in the eye, travel to high altitude locations and air travel should be avoided, as the bubble will expand, causing injury to the eye. Similarly, nitrous oxide anesthetic causes bubble expansion and secondary ocular injury.
As with all ocular surgeries, there is a risk of infection called endophthalmitis. However, this rarely occurs.
From the Expert…
During my career, macular holes have gone from an untreatable disease to one which is almost always repairable. Surgical success has improved over time with advancements in surgical techniques and equipment. In my opinion, peeling the ILM, achievable with the use of intraocular dye, has greatly increased the rate of successful hole closure.
Complications can usually be avoided with careful technique. Eye pressure abnormalities can occur postoperatively and are usually managed with drops, or occasionally, by removing some of the gas bubble. Retinal tears are best detected intraoperatively where they can be treated with laser. The risk for recurrence of the hole following surgical repair can be minimized with ILM removal. Finally, patient compliance with head positioning is critical for successful macular hole closure.
ADDITIONAL RESOURCES
American Academy of Ophthalmology Retina/Vitreous Panel. Preferred Practice Pattern® Guidelines. Idiopathic Macular Hole. San Francisco, CA: American Academy of Ophthalmology; 2014. Available at: www.aao.org/ppp.
Gupta, O. Macular Hole. American Academy of Ophthalmology. EyeWiki. https://eyewiki.aao.org/Macular_Hole. Accessed July 24, 2019.
Retina Health Series. Macular Hole. The Foundation of the American Society of Retina Specialists. https://www.asrs.org/content/documents/fact_sheet_2_macular_hole_new.pdf. Accessed July 24, 2019.
Summary Benchmarks for Preferred Practice Pattern® Guidelines. Idiopathic Macular Hole. American Academy of Ophthalmology; 2018.

