Paradigm Shift: Anti-VEGF Therapy in the Treatment of Diabetic Eye Disease
Please see the previous blog, Diabetic Retinopathy, for more information on diabetic eye disease.
The treatment for diabetic retinopathy was greatly improved with the introduction and refinement of laser photocoagulation in the 1970’s and 80’s. While laser treatment is effective in limiting vision loss, only a minority of patients achieve improvement of vision. For decades, laser treatment was the undisputed standard of care.
Paradigm Shift
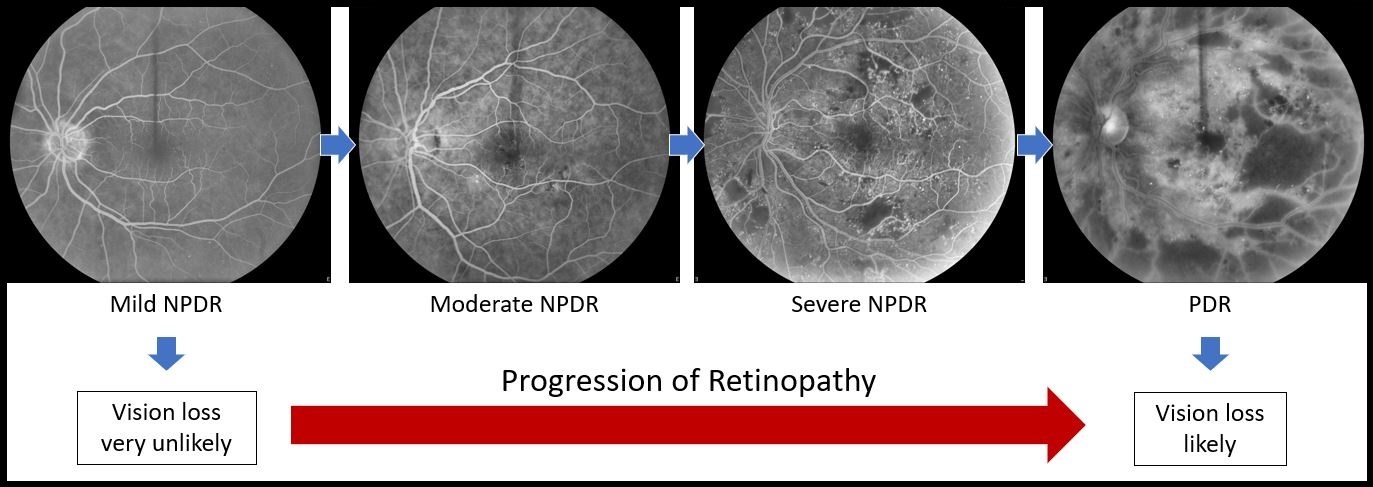
Vision loss from diabetic retinopathy is related to the severity of the disease. In mild NPDR, the risk for vision loss is low. As the disease worsens, the risk for loss of vision increases.
In recent years, anti-VEGF injections have been utilized to treat patients with diabetic macular edema. While treating diabetics for edema with anti-VEGF therapy, an improvement in the diabetic retinopathy is frequently observed.
Studies analyzing the effect of anti-VEGF therapy for diabetic retinopathy have shown the occurrence of a vision threatening event in two years decreased from 41% to 10% in the treatment group. There was also a decrease in the severity of the disease. Therefor, with the administration of anti-VEGF treatment, the severity of retinopathy as well as associated vision threatening events has been shown to decrease. To take advantage of this benefit, diabetic patients with retinopathy, but without macular edema, have now been approved for anti-VEGF therapy.
Complications
Risks of intravitreal injections are uncommon, though may be severe, and include infection, hemorrhage, and retinal detachment. Monitoring for complications is necessary to avoid loss of vision, and patients should be educated on the warning signs. Patients who experience loss of vision, severe pain, light sensitivity, and/or new floaters following treatment, should be evaluated promptly.
From the Expert…
Anti-VEGF injections for the treatment of diabetic retinopathy is a great advancement. The treatment protocol varies from doctor to doctor, and from patient to patient. I prefer to initiate treatment at 2-3 month intervals and continue for a minimum of 2-3 years. Clinical improvement is monitored by performing angiograms which provide details about the disease severity. Electroretinograms (ERG) may be useful to assess the physiologic health of the retina.
Finally, and most importantly, the satisfied patient, describing a noticeable improvement in their vision, is the best measure of therapeutic success!
Additional Resources
Gross JG, Glassman AR, Liu D, Sun JK, Antoszyk AN, Baker CW, Bressler NM, Elman MJ, Ferris FL, Gardner TW, Jampol LM, Martic DF, Melia M, Stockdale CR, Beck RW, Diabetic Retinopathy Clinical Research Network. Five-Year Outcomes of Panretinal Photocoagulation vs Intravitreous Ranibizumab for Proliferative Diabetic Retinopathy: A Randomized Clinical Trial. JAMA Ophthalmol 2018;136:1138-1148.
Wykoff CC, Eichenbaum DA, Roth DB, Hill L, Fung AE, and Haskova Z. Ranibizumab Induces Regression of Diabetic Retinopathy in Most Patients at High Risk of Progression to Proliferative Diabetic Retinopathy. Ophthalmology Retina 2018;2:997-1009.
Retina Health Series. Intravitreal Injections. The Foundation of the American Society of Retina Specialists. https://www.asrs.org/content/documents/fact-sheet-30-intravitreal-injections.pdf. Accessed July 31, 2019.